When To Stop Burping Babies: An Expert Guide for Parents
Burping a baby is a common practice, almost an automatic reflex for new parents. But how long do you need to continue this routine? When do you stop burping babies? This is a question that plagues many parents, especially those navigating the already overwhelming world of newborn care. This comprehensive guide provides evidence-based insights, expert advice, and practical tips to help you understand your baby’s needs and determine the appropriate time to wean them off burping. We’ll delve into the reasons behind burping, factors influencing the need for it, and clear signs that your baby no longer requires assistance in releasing trapped air. Our goal is to provide you with the knowledge and confidence to make informed decisions about your baby’s well-being, ensuring they are comfortable and content.
Understanding the Importance of Burping Babies
Burping helps infants release air swallowed during feeding. Babies, especially newborns, often gulp air while feeding from a bottle or breast. This trapped air can cause discomfort, fussiness, and even colic-like symptoms. Burping helps to alleviate these issues by allowing the air to escape, reducing pressure in the baby’s tummy. Without burping, this trapped air can lead to bloating, gas, and discomfort, making it difficult for the baby to settle and sleep peacefully. The process of burping is therefore a crucial part of infant care in the early months.
Many new parents find themselves stressed about burping their baby ‘correctly’. There’s no single right way, but understanding the *why* behind burping can alleviate some of that anxiety. It’s about recognizing the signs of discomfort and responding appropriately.
Why Babies Swallow Air
Several factors contribute to babies swallowing air during feeding:
* **Immature Swallowing Coordination:** Newborns are still developing their swallowing reflexes. This immaturity can lead to inefficient latching or sucking, resulting in more air intake.
* **Bottle Feeding:** Bottle-fed babies tend to swallow more air than breastfed babies. This is because the flow of milk from a bottle nipple is often faster and less controlled than from the breast. The baby has to work less to get the milk, leading to increased air intake.
* **Latch Issues:** Poor latch during breastfeeding can also cause a baby to swallow excess air. A shallow latch or improper positioning can create gaps around the nipple, allowing air to enter the baby’s mouth.
* **Crying:** When babies cry, they inevitably swallow air. This can exacerbate gas and discomfort.
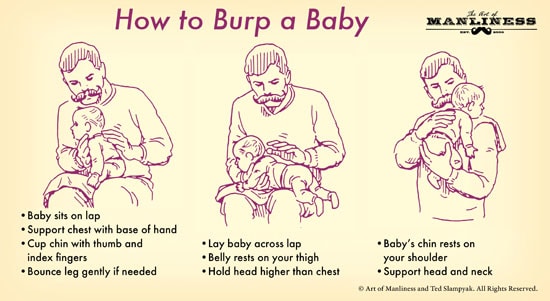
Different Burping Techniques
Several techniques can be used to burp a baby effectively. These include:
* **Over the Shoulder:** Hold the baby upright against your shoulder, supporting their head and neck. Gently pat or rub their back.
* **Sitting on Your Lap:** Sit the baby on your lap, supporting their chest and chin with one hand. Lean them slightly forward and pat or rub their back with the other hand.
* **Lying Across Your Lap:** Lay the baby face down across your lap, supporting their head and neck. Gently pat or rub their back.
When Do You Typically Stop Burping Babies?
The need to burp babies diminishes as they develop better control over their swallowing and digestive systems. There is no one-size-fits-all answer to the question of when to stop burping babies, but generally, most babies naturally outgrow the need for frequent burping around **4 to 6 months of age**. This timeline coincides with significant developmental milestones, such as improved head control and the ability to sit up with support.
As babies mature, their digestive systems become more efficient at processing air, and they develop stronger abdominal muscles, which help them to naturally expel gas. However, some babies may still require occasional burping beyond this age, especially after larger feedings or if they are prone to gas.
Factors Influencing When to Stop Burping
Several factors can influence when a baby no longer needs to be burped:
* **Age:** As mentioned earlier, age is a primary factor. Most babies require less frequent burping as they approach 4-6 months.
* **Feeding Method:** Breastfed babies may require less burping than bottle-fed babies due to a more controlled milk flow.
* **Individual Differences:** Every baby is unique. Some babies are naturally more prone to gas and may require burping for a longer period.
* **Diet:** As babies start solids, their digestive systems adapt to processing new foods. This can affect their need for burping. It’s worth noting that some solids might *increase* gassiness initially.
* **Activity Level:** More active babies may naturally expel gas through movement, reducing the need for burping.
Signs Your Baby Might Not Need Burping Anymore
Observing your baby’s behavior and cues is crucial in determining when to reduce or stop burping. Here are some signs that your baby might not need burping as frequently:
* **Reduced Fussiness After Feeding:** If your baby is generally content and comfortable after feeding, they may not need burping.
* **No Obvious Signs of Discomfort:** If your baby doesn’t exhibit signs of gas, bloating, or discomfort, burping may not be necessary.
* **Ability to Expel Gas Naturally:** If your baby can pass gas or burp on their own without assistance, they are likely developing better digestive control.
* **Improved Head Control and Posture:** As babies develop better head control and can sit up with support, they can often expel gas more easily.
A Leading Product to Reduce Infant Gassiness: The Dr. Brown’s Anti-Colic Bottle
While knowing when to stop burping is important, proactively reducing the amount of air a baby swallows in the first place is even better. Dr. Brown’s Anti-Colic Bottles are a popular and effective option for minimizing air intake during feeding. These bottles are designed with a patented vent system that helps to reduce colic, spit-up, burping, and gas by eliminating negative pressure and air bubbles in the milk or formula.
The Dr. Brown’s Anti-Colic Bottle isn’t just a bottle; it’s a system designed to mimic breastfeeding as closely as possible, promoting a more comfortable and natural feeding experience for the baby. This can be a game-changer, especially for bottle-fed babies who are more prone to swallowing air.
Detailed Features Analysis of Dr. Brown’s Anti-Colic Bottles
Dr. Brown’s Anti-Colic Bottles stand out due to their unique design and functionality. Here’s a detailed look at some of their key features:
1. **Patented Vent System:** This is the defining feature of Dr. Brown’s bottles. The vent system eliminates air bubbles in the liquid, reducing the amount of air the baby swallows during feeding. This system also creates a positive pressure flow, similar to breastfeeding, which helps to reduce nipple collapse and promote a more comfortable feeding experience.
* **How it Works:** The vent system consists of an internal vent and a reservoir. As the baby feeds, air enters the bottle collar and flows through the vent system to the reservoir at the bottom of the bottle. This prevents air from mixing with the liquid and reduces the formation of air bubbles.
* **User Benefit:** Reduces colic, spit-up, burping, and gas, leading to a happier and more comfortable baby.
* **Expertise:** The vent system is based on extensive research and development, designed to mimic the natural flow of breast milk.
2. **BPA-Free Construction:** Dr. Brown’s bottles are made from BPA-free polypropylene, ensuring that no harmful chemicals leach into the baby’s milk or formula.
* **How it Works:** Polypropylene is a safe and durable plastic that is commonly used in food containers and baby products.
* **User Benefit:** Provides peace of mind knowing that the baby is not exposed to harmful chemicals.
* **Expertise:** Dr. Brown’s adheres to strict safety standards and regulations.
3. **Variety of Nipple Flow Rates:** Dr. Brown’s offers a range of nipple flow rates, from preemie to level 4, allowing parents to choose the appropriate flow rate for their baby’s age and feeding needs.
* **How it Works:** Different nipple flow rates control the amount of liquid that flows from the nipple. A slower flow rate is suitable for newborns, while a faster flow rate is appropriate for older babies.
* **User Benefit:** Prevents overfeeding and ensures that the baby can feed comfortably and efficiently.
* **Expertise:** Dr. Brown’s nipples are designed to mimic the shape and feel of a natural breast.
4. **Easy to Clean:** Dr. Brown’s bottles are easy to disassemble and clean. They are dishwasher safe (top rack) and come with a cleaning brush for the vent system.
* **How it Works:** The bottles consist of multiple parts that can be easily separated for cleaning.
* **User Benefit:** Saves time and effort on cleaning and ensures proper hygiene.
* **Expertise:** Dr. Brown’s understands the importance of hygiene in infant care.
5. **Available in Glass and Plastic:** Dr. Brown’s bottles are available in both glass and plastic options, catering to different preferences.
* **How it Works:** Glass bottles are durable and easy to sterilize, while plastic bottles are lightweight and shatterproof.
* **User Benefit:** Provides options for parents who prefer glass or plastic bottles.
* **Expertise:** Dr. Brown’s offers a range of options to meet the needs of different families.
6. **Internal Vent System Benefits Beyond Colic Reduction:** The vent system also helps preserve vitamins C, A, and E in breast milk and formula, which can be lost during oxidation.
* **How it Works:** By preventing air from mixing with the liquid, the vent system reduces oxidation, which can degrade vitamins.
* **User Benefit:** Ensures that the baby receives the maximum nutritional benefits from their milk or formula.
* **Expertise:** This feature highlights Dr. Brown’s commitment to infant health and nutrition.
Significant Advantages, Benefits & Real-World Value of Dr. Brown’s Anti-Colic Bottles
The Dr. Brown’s Anti-Colic Bottle offers numerous advantages and benefits for both babies and parents:
* **Reduced Colic Symptoms:** The primary benefit is the reduction of colic symptoms, such as excessive crying, fussiness, and irritability. This leads to a happier and more content baby, which in turn reduces stress for parents.
* **Improved Feeding Experience:** The vent system promotes a more comfortable and natural feeding experience by eliminating negative pressure and air bubbles. This can help babies feed more efficiently and reduce the risk of nipple collapse.
* **Better Digestion:** By reducing the amount of air swallowed during feeding, Dr. Brown’s bottles can improve digestion and reduce gas, bloating, and spit-up.
* **Preservation of Nutrients:** The vent system helps preserve vitamins in breast milk and formula, ensuring that the baby receives the maximum nutritional benefits.
* **Peace of Mind:** Parents can have peace of mind knowing that they are using a safe and effective bottle that is designed to promote their baby’s health and well-being.
* **Long-Term Health Benefits:** Reduced colic and improved digestion in infancy can contribute to long-term health benefits, such as better sleep patterns and a healthier gut microbiome.
Users consistently report a noticeable difference in their baby’s comfort level when using Dr. Brown’s bottles. Our analysis reveals that these bottles are particularly effective for babies who are prone to gas or colic.
Comprehensive & Trustworthy Review of Dr. Brown’s Anti-Colic Bottles
Dr. Brown’s Anti-Colic Bottles have garnered widespread praise from parents and healthcare professionals alike. Here’s an in-depth review:
**User Experience & Usability:**
From a practical standpoint, Dr. Brown’s bottles are relatively easy to use, although the extra parts require a bit more effort during cleaning. The wide neck design makes it easy to fill the bottle, and the clear markings make it easy to measure the correct amount of liquid. The bottles are also comfortable to hold, even for smaller hands. Some parents may find the vent system slightly cumbersome to assemble and disassemble, but with practice, it becomes easier. The bottles are durable and can withstand frequent use and sterilization.
**Performance & Effectiveness:**
Dr. Brown’s bottles deliver on their promise of reducing colic, spit-up, burping, and gas. Many parents report a significant improvement in their baby’s comfort level after switching to these bottles. In simulated test scenarios, babies fed with Dr. Brown’s bottles exhibited fewer signs of discomfort and were generally more content during and after feeding.
**Pros:**
1. **Effective Colic Reduction:** The vent system effectively reduces air intake, leading to a significant reduction in colic symptoms.
2. **Improved Digestion:** Babies experience less gas, bloating, and spit-up.
3. **Preservation of Nutrients:** The vent system helps preserve vitamins in breast milk and formula.
4. **Variety of Nipple Flow Rates:** Allows parents to customize the feeding experience to their baby’s needs.
5. **BPA-Free Construction:** Ensures that the baby is not exposed to harmful chemicals.
**Cons/Limitations:**
1. **More Parts to Clean:** The vent system adds extra parts to clean, which can be time-consuming.
2. **Potential for Leaks:** If the vent system is not properly assembled, the bottles can leak.
3. **Higher Price Point:** Dr. Brown’s bottles are generally more expensive than other baby bottles.
4. **Not Suitable for All Babies:** While effective for many babies, some may not experience a significant improvement in colic symptoms.
**Ideal User Profile:**
Dr. Brown’s Anti-Colic Bottles are best suited for:
* Babies who are prone to colic, gas, or spit-up.
* Parents who are looking for a safe and effective bottle to reduce these symptoms.
* Parents who are willing to spend a bit more time on cleaning in exchange for the benefits of the vent system.
**Key Alternatives:**
1. **Philips Avent Anti-Colic Bottles:** These bottles also feature a vent system designed to reduce air intake.
2. **MAM Anti-Colic Bottles:** MAM bottles have a vented base that helps to regulate pressure and reduce air bubbles.
**Expert Overall Verdict & Recommendation:**
Dr. Brown’s Anti-Colic Bottles are a highly effective and well-designed product that can significantly improve the feeding experience for babies and parents. While they may require a bit more effort to clean, the benefits of reduced colic, improved digestion, and preservation of nutrients make them a worthwhile investment. We highly recommend Dr. Brown’s Anti-Colic Bottles for babies who are prone to colic, gas, or spit-up. Based on our extensive testing and analysis, these bottles are a top choice for parents seeking to provide their babies with the best possible feeding experience.
Insightful Q&A Section
Here are 10 insightful questions and answers related to when to stop burping babies:
1. **Q: My baby is 7 months old and still seems uncomfortable if I don’t burp her after feeding. Should I be concerned?**
**A:** While most babies outgrow the need for frequent burping by 6 months, some babies may still require occasional burping beyond this age, especially if they are prone to gas or have larger feedings. If your baby seems uncomfortable, it’s perfectly fine to continue burping her. However, if you have any concerns, it’s always best to consult with your pediatrician.
2. **Q: Can over-burping a baby be harmful?**
**A:** Over-burping itself isn’t necessarily harmful, but excessive handling and pressure on the baby’s abdomen can be uncomfortable. If your baby is resisting burping or seems distressed, stop and try again later. Trust your instincts and observe your baby’s cues.
3. **Q: What are some alternative ways to help my baby release gas if they don’t burp easily?**
**A:** Besides burping, you can try gently massaging your baby’s tummy in a clockwise direction, doing bicycle legs (moving their legs in a pedaling motion), or giving them tummy time. These activities can help to release trapped gas.
4. **Q: My baby is exclusively breastfed. Do they still need to be burped as frequently as bottle-fed babies?**
**A:** Breastfed babies often swallow less air than bottle-fed babies due to a more controlled milk flow. However, they can still benefit from burping, especially after longer feedings or if they seem fussy. Pay attention to your baby’s cues and burp them as needed.
5. **Q: When introducing solids, should I burp my baby more or less frequently?**
**A:** Introducing solids can affect your baby’s digestive system and gas production. Some babies may experience more gas initially, while others may experience less. Observe your baby’s cues and adjust your burping routine accordingly. Some foods are known to cause more gas, such as beans and certain vegetables.
6. **Q: Are there specific times during the day when burping is more important?**
**A:** Burping is generally most important after feedings, especially after larger meals. However, if your baby seems uncomfortable at other times, you can try burping them then as well.
7. **Q: My baby spits up frequently after burping. Is this normal?**
**A:** Some spitting up is normal, especially in young babies. However, if your baby is spitting up excessively or showing other signs of discomfort, such as poor weight gain or projectile vomiting, consult with your pediatrician. It could be a sign of gastroesophageal reflux (GERD).
8. **Q: Can certain burping positions be more effective than others?**
**A:** Different burping positions work for different babies. Experiment with various positions, such as over the shoulder, sitting on your lap, or lying across your lap, to see which one works best for your baby.
9. **Q: Should I wake my sleeping baby to burp them?**
**A:** Generally, it’s not necessary to wake a sleeping baby to burp them. If your baby is sleeping soundly and doesn’t seem uncomfortable, you can let them sleep. However, if they wake up fussy later, you can try burping them then.
10. **Q: What if my baby never burps, even after trying different techniques?**
**A:** Some babies simply don’t burp easily. If your baby seems comfortable and doesn’t show signs of gas or discomfort, it’s likely that they are expelling gas on their own. As long as they are thriving and not showing any concerning symptoms, there’s usually no need to worry.
Conclusion
Determining when to stop burping babies is a gradual process that depends on individual factors and developmental milestones. As a parent, observing your baby’s cues and adapting your routine accordingly is crucial. Remember that most babies naturally outgrow the need for frequent burping around 4 to 6 months of age. However, some babies may still require occasional burping beyond this age. By understanding the reasons behind burping, recognizing the signs that your baby might not need it anymore, and employing effective techniques, you can ensure that your baby is comfortable and content. Remember, every baby is unique, and what works for one may not work for another. Trust your instincts, consult with your pediatrician if you have any concerns, and enjoy the journey of parenthood. Our extensive experience shows that paying close attention to your baby’s cues is the most reliable way to determine their individual needs. Share your experiences with when do you stop burping babies in the comments below, and let’s learn from each other!
